
Eyesight Ophthalmic Services have been in the forefront of vision correction for over 20 years now. We offer unmatched experience utilizing the best available technology in cataract surgery including the latest in intraocular lens (“IOLs”) that will work best for your vision correction needs. Today’s procedures offer shorter recovery times, are virtually painless, and the improvement in your vision will be almost immediate.
The types of lenses available today are so advanced that they are even attracting those individuals who don’t have cataracts, but want to reduce their dependence on glasses for all ranges, such as distance, intermediate, and near ranges. This can often eliminate the need for glasses and, even, bifocals.
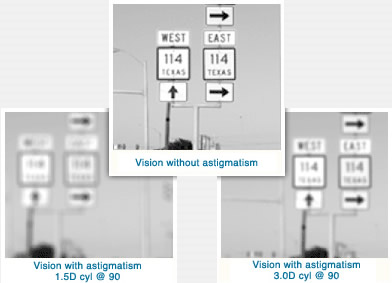
Toric IOL is a special intraocular lens (“IOL”) created for cataract patients who suffer from astigmatism and is an option for some cataract patients who want to correct astigmatism without undergoing additional surgery. That means a faster, more predictable, and comfortable recovery than ever before.
The Toric IOL is generally used in conjunction with cataract surgery. Cataracts are opacities that form in the eye’s crystalline (natural) lens and are caused by a breakdown of tissue and accumulation of proteins that make the lens cloudy. Over time, cataracts cloud the lens and keep light from reaching the retina, creating impaired, blurred vision.
The only treatment that removes cataracts is cataract surgery, which involves removing the natural lens of the eye and replacing it with an intraocular lens (IOL).
A Toric IOL is used to treat cataract patients who want to correct astigmatism without undergoing additional surgery. The toric lens will remain in the eye for life and will need no particular care. It will simply be a part of your eye.
The following information answers questions that we frequently hear from our patients about the Toric IOL however, some of these questions also apply to Cataract Surgery and other intraocular lenses (IOLs) including: Tecnis and Crystalens. For more information, please contact us.